Vascular Trauma
 This is one of the common emergencies worldwide. A basic understanding of the blunt and penetrating injuries to the extremities and the complications helps minimise mortality and morbidity.
This is one of the common emergencies worldwide. A basic understanding of the blunt and penetrating injuries to the extremities and the complications helps minimise mortality and morbidity.
Pathophysiology
The vascular tree has some limited protection from stretching and bending leading to fewer blunt injuries involving vessels. The smooth muscle in the wall of the artery protects from stretch and minor puncture which heal spontaneously in most cases. The smooth muscle also protects from death due to ongoing bleeding. If the artery is transacted, vascular spasm along with low pressure due to hemorrhage promotes clotting at the site of injury to preserve vital supply and perfusion to the vital organs.
In the upper limb the axilla, upper and medial aspect of the arm and the anticubital fossa are more prone because of the superficial nature. Below the elbow there are minimal chances of ischemia if the ulnar or the radial arteries are intact along with the palmer arch. In 95% results are good.
In the lower extremity the areas of injury are mainly groin thigh and popliteal fossa. The injuries below the knee do not lead to ischemia because the popliteal artery trifurcates into 3 – the anterior and posterior tibials and the peroneal. Thus if one is injured the other 2 are adequate to maintain circulation. In modern combat the injuries from high velocity gun shots and blasts are much more serious than pistol shots and stab injuries.
Modern injuries are 5 times as serious as injuries of the past. Knee injuries and gunshot injuries are more likely to involve vessels.
Causes
- Gunshot injuries – 70 – 80% need intervention.
- Stab injuries – 5-10 % need intervention.
- Blunt trauma – the account for only 10% of the injuries but because of the concomitant soft tissue injury the chances of amputation is higher.
- Latrogenic injuries account for 10% and cardiac catheterization and central line insertions need surgical intervention. These injuries are on the rise.
Presentation

Crush injury foot medial view with avulsion of the sole
Peripheral injuries account for 80% of all vascular injuries and 2/3rd of the vascular injury cases involve the lower limb. Penetrating injuries account for 70 – 90% of vascular injuries. Iatrogenic vascular injuries are in the increase when done diagnostically or therapeutically. 90% of the peripheral vascular injuries are in males between 20 – 40 years.
Increasing hemorrhage needing resuscitation is an indication for operative exploration. Vascular injuries are classified clinically into hard and soft injuries depending on the examination:
The hard signs include
- Observed pulsatile bleeding.
- Arterial thrill on palpation.
- Bruit on auscultation.
- Signs of distal ischemia.
- Visible expanding hematoma.
The soft signs are a cool, pulseless leg which could be due to low blood pressure. If there is normal pulse in the other leg it is a sign of vascular injury on the affected side. Neurological deficit, delayed capillary filling and bony abnormality calls for further tests including angiography and possible surgical exploration and repair.
Thus the soft signs include:
- History of significant hemorrhage.
- Reduced pulse volume compared to the contralateral side.
- Bony injury or penetrating wound.
- Neurological deficit.
The hard and soft signs determine the need for Doppler study and angiography. ABI is another helpful non-invasive test.
Indications
Hard signs like absent pulse and the reduced pulse volume are indications for further tests like arteriogram and exploration in the OT. The softer signs like temperature change, colour change, capillary filling and neurological deficit demands close observation and monitoring. If ABI is > 0.9 it calls for observation while < 0.9 calls for further tests like Doppler study. Angiogram in stable cases while exploration in unstable cases is recommended.
- Relevant Anatomy
- It is most vital to know the surgical anatomy to locate vessels that are not palpable and have o pulse due to arterial injury. The anatomy of the vessels, bone muscle and their relationships is essential to minimise the incision length and surgical tissue dissection. Ongoing hemorrhage makes tissue planes difficult to recognise and the artery and vein retract into the depths of the wounds.
- Temporary control is possible by proximal pressure but in exsanguination one may have to apply tourniquet. However in cases where tourniquet is applied there is a markedly high incidence of amputation in the injured extremity. Tourniquet can save live but results in loss of limb.
- Contraindications
- If patient has renal failure the contrast dye for angiography is contraindicated. To minimise the chances of renal failure volume is given along with sodium bicarbonate. Persistent hemorrhage and hemodynamic instability are contraindications to all investigations and indication of surgical exploration. Colour Doppler studies are indicated if angiography is contraindicated.
- Laboratory Studies
- Blood tests – CBC, platelets, urea, createnine, sodium, potassium blood sugar, PT and PTT. Cross match 4-8 units depending on the severity of injury. In acute hemorrahge the hematocrit and haemoglobin are within normal range despite significant blood loss.

X-Ray showing fracture both
bones forearm - Imaging studies
- Plain X-Ray to see for any fractures or dislocations
- CT scan for bony and soft tissue anatomy as a diagnostic modality but not vascular injuries. CT scan should not be used except in unusual circumstances.Angiography is used in stable patients without renal complications. Renal functions are done before this test is carried out. On-table angiogram is preferred by many but surgeon must know the renal function and be familiar with the dye load to be safely given.Colour Doppler studies are very valuable in experienced hands and could be done in the OT.
- Ankle-Brachial index – this determines vascular insufficiency but not the site of injury. ABI approaches the accuracy of angiograms in determining arterial injury and the need for intervention.Assessing the Doppler signal in peripheral vessles is more sensitive than manual palpation and helps assessing total occlusion or transaction of artery.
Staging
The Mangled Extremity Severity Score (MESS) has been used to decide for extremity amputation but not at the expense of clinical assessment. A MESS score of 7 has been used as a cut-off point for amputation prediction. All patients with MESS score < 7 were safe and did not need amputation. Amputation was also avoided in many patients with MESS > 7. The decision to amputate should be based on clinical signs and intra-operative findings of irreversible limb ischemia.
Medical Therapy
This is not an option if hard signs are present. It mainly applies to patients who are asymptomatic or have only soft signs. These patients are kept under observations and if the soft signs change to hard signs then surgical intervention is needed. Antiplatelet drugs and anticoagulants are needed if synthetic grafts are inserted but there is a possibility of bleeding in other traumatised tissue and may be a potential threat if there is head injury or spine injury.
Surgical Therapy

Fracture stabilization of forearm bones
This could be limited to exploration of the vessels only or performing a major reconstruction or a bypass. The timing of surgical intervention is critical to the outcome in vascular injuries. Vascular reconstruction within first 3 hours has the best outcome. Always stabilize the bony fragments before performing vascular repair.
If injured segment is < 1 cm it is possible to mobilise the artery at either end and perform an end to end anastamosis. There must be no traction on the artery to bring it together. Minimal surrounding dissection must be done to avoid devitalizing the surrounding tissue. In very severe injuries it may be impossible to do any correction and the only option may be ligation of the bleeding artery. In this case survival would depend on presence of collaterals, pre-existing atherosclerotic disease, competent venous flow and volume status.
Venous ligation in the popliteal vein carries a higher possibility of amputation than femoral or external iliac vein ligation. A patient with severe head injury may not be able to stand lengthy vascular repair and so the only option would be ligation. Vasoconstriction must be minimised post-operatively. Removal of the dead tissue due to the injury (debridement) may have to be carried out.

After debridement a healthy
clean wound
If patient condition allows and prolonged procedure is possible then autologous vein bypass is done using saphenous or cephalic vein from same or other side. PTFE is used mainly for above knee or above elbow bypasses. PTFE has been used successfully in contaminated fields with low infection rates for venous and arterial reconstruction.
At the completion of the surgery one should anticipate reperfusion injury and compartment syndrome. Compartment syndrome occurs when the perfusion of the limb suffers for over 6 hours. The treatment of compartment syndrome is fasciotomy which carries a risk of infection, fluid and blood loss and may need skin graft or skin closure at a later date. These complications have been weighed against risk of limb loss, renal failure from myoglobulin release and tissue gangrene. Prophylactic fasciotomies are recommended despite the side effects in severe cases. The most challenging injuries are the crush injuries involving the bones, soft tissue and vascular tissue. They carry an extremely high risk of amputation.
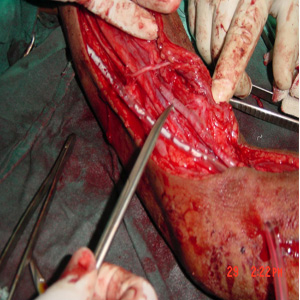
Vein bypass shown and pointed out
The Mangled Extremity Severity score (MESS) is widely used scoring system and includes 1) degree of soft tissue and skeletal injury 2) limb ischemia 3) patient age 4) shock. Interventional radiological techniques like embolization for complications like pseudoaneurysms and AV malformation are performed. Stenting are done in some centres but long term follow-up are not known.

Fasciotomy – exposing muscles to
remove internal pressure
The Mangled Extremity Severity score (MESS) is widely used scoring system and includes 1) degree of soft tissue and skeletal injury 2) limb ischemia 3) patient age 4) shock. Interventional radiological techniques like embolization for complications like pseudoaneurysms and AV malformation are performed. Stenting are done in some centres but long term follow-up are not known.
Pre-operative details
If reconstruction is planned then the best results are obtained in stable patients with normal lab findings and pre-operative angiography to localize the lesion. In cases to save life all investigation details are bypassed and hemorrhage control done.
Intra-operative details
In life threatening bleeding only ligation of the bleeder may be possible to stabilize the patient. One has to make a decision whether to save the limb but this should not be done at the cost of life.
Post-operative details
Frequent monitoring and vascular checks are carried out in the first 48 hours. Anticoagulation and antiplatelets may be indicated but have to be balanced against fatal hemorrhage from other injuries. Maintain adequate hydration and a good urine output of over 50/hr.
Follow-up
Vascular repair with normal pulses does not need angiogram. A colour Doppler study is needed to chart the flow of blood.
Complications
Graft thrombosis is the commonest due to vessel narrowing after repair or kinking of the graft. Ligation of the vessel may lead to amputation. Nerve injury may pose a major problem if not recognised in time. This could lead to a useless limb causing more problems than an amputation.

Gangrenous amputation stump
Outcome and prognosis
Death solely due to vascular injuries is rare though it may occur due to exsangunation and myocutaneous infection (sepsis). Major venous injury accompanies 13 – 51% major arterial injury. Despite successful vascular repair if the nerve has been damaged it leads to an insensate limb which may be wiser to amputate. There may be no early amputations but the late amputation rate is > 40%. The results are not good where vascular injuries are accompanied with soft tissue, nerve and bone injuries. Early vascular repair improves the outcome but cannot reverse the effects of some injuries. Amputation and disability rates remain high even with early transport, trauma care and operative intervention.
Future and controversies
Improvement of Emergency medical services, faster transport, and other advances in interventional radiology may help further reduce the mortality and the morbidity in extremity vascular injuries. However lies in prevention of these types of accidents like safer motorcycles, enforcement of speed limits and injury prevention programs.