Pulmonary Embolism ( PE )
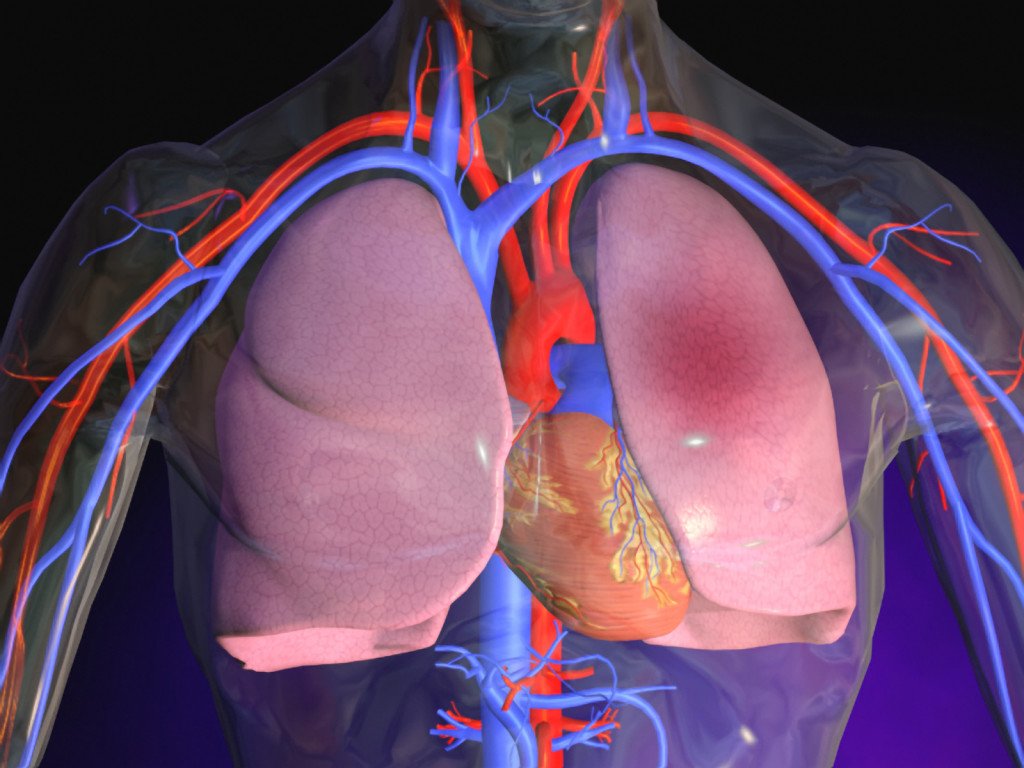
The lungs are organs in the chest which contain sacks that are very thin and filled with air that we breath from outside. The walls of these sacs are called membranes and contain the thinnest of vessels called capillaries. The distance between the air in the sacs and the blood is very small and air passes into the vessels containing blood. Thus oxygenation takes place.
Blood travels throughout the body in two types of vessels – arteries and veins. The former takes blood from the heart to the tissues of the body to deliver the oxygen while the carbon dioxide which is the waste product travels in the veins back to the heart and then the lungs.
Heart is a dual chamber – the left pumps the oxygenated blood to the tissues while the left side pumps the deoxygenated blood back to the lungs to be oxygenated. Since the blood goes in circles it is called circulation.
A clot that forms in the veins can break off and travel to the lungs via the right side of the heart and lodge in the branches of the pulmonary tree. A clot that travels from one part of the body via the circulation is called an embolus. Since it travels to the lungs it is called pulmonary embolus (PE). This embolus lodging in the pulmonary artery prevents the exchange of oxygen and also stops the circulation to the lung tissue – infarction of the lung.
PE should always be considered in every case of shortness of breath and is one of the life threatening causes of chest pain. Non thrombus causes of PE include:
- Fat embolism from fracture femur.
- Amniotic fluid embolism in pregnancy.
- Tumour tissue from cancer.
- Presentation is same as in case of blood clot.
Causes and risk factors for PE
PE is the end result of deep vein thrombosis in the deep venous system. The commonest site is the legs though it could arise from any other site. The risk factors for PE are the same as for DVT and are referred to as Virchow’s triad. These include:
- Prolonged immobilization which alters the normal blood flow – stasis.
- Increased clotting potential of the blood (hypercoagulability).
- Damage to the vein walls.
Prolonged immobilization
- Extended travel – sitting in car, plane or train.
- Hospitalization or prolonged bed rest.
Increased clotting potential
- Medication – birth control pill, estrogens.
- Smoking.
- Genetic predisposition.
- Polycythemia.
- Cancer.
- Pregnancy & upto 6-8 weeks post-partum.
- Surgery.
Vessel wall damage
- Prior venous thrombosis.
- Trauma to the lower leg with or without surgery.
Signs & symptoms
- Complains of chest pain and breathlessness. Pain is pleuritic and increases on deep breathing. There may be bloody sputum in cough.
- Patients have stable signs though there is increased pulse rate.
- Severe PE may give rise to shock or cardiac arrest in the case of massive saddle embolus. The heart rate and respiratory rate are elevated.
- Oxygen saturation may be decreased.
- Patient could be light headed and cyanosed.
- In very severe cases the patient collapses, stops breathing and the heart stops beating – he is dead.
Diagnosis

There has to be a suspicion that PE may be the cause of chest pain and breathlessness. There may be a history of DVT in the legs. The condition may be confused with heart attack, pneumonia, pneumothorax or dissecting thoracic aneurysm.
Chest examination is mostly normal though there may be a pleural rub. This is because the pleura is full of nerve endings and the inflammation caused by PE makes it very painful especially on deep breathing.
One must look for DVT in the legs – warmth, swelling, redness & tenderness. It is very important to note that the signs associated with DVT may be completely absent in the presence of clot.
Blood tests - CBC electrolytes, BUN & createnine.
Chest X-Ray - mostly normal.
ECG – mostly normal though sinus tachycardia (HR > 100 bpm). In advanced cases there may be right heart strain.
Since the cost of missing PE can lead to death of the patient, one must be very persistent to exclude PE.
Pulmonary Angiogram - this is the gold standard. With this invasive test the dye shows filling defects in the pulmonary arteries.
d-Dimer blood test – this test measures one of the break-down products of a blood clot. If the test is normal then the likelihood of PE is very low. This test is not specific for blood clots in the lungs and may be positive in pregnancy, injury, recent surgery or recent infection.
CT Scan with contrast shows filling defects in the pulmonary arteries. There is always a risk of allergic reaction to the dye, and derangement of the renal function. Though we avoid radiation exposure in pregnancy however the risk of death in PE is so high that we perform CT after the first trimester.
Ventilation-perfusion scan (V/Q Scan) - here we use labelled chemicals in inhailed air into lungs and match it with blood flow in the arteries. Mismatch happens if there is good air entry but no blood flow. These tests are not fool proof and there is a 5% possibility of PE in low probability V/Q scan.
Venous Doppler study – this looks for leg clots (DVT). If positive for DVT then we are reasonably certain that chest pain and shortness of breath is due to PE.
Echocardiogram is done if ECG shows strain on the right heart.
Treatment
The best treatment for PE is prevention by minimizing the risk of DVT. In case of small PE, if the patient is hemodynamically stable and who is complaint with treatment, can be sent home with close OPD follow-up. Those who are unstable need hospitalization.
- Anticoagulation – low molecular weight heparin (LMWH) and warfarin (coudamin) are started right away because oral warfarin takes 1 week to take effect. Since warfarin can thin the blood so much that it can cause bleeding, it needs very careful monitoring.
- If a patient has renal failure LMWH is not metabolised, then IV heparin can be used as a first step after being hospitalized as regular monitoring is done with blood tests. Anticoagulation is given for a minimum of 6 months. Warfarin is monitored via blood prothombin time (PT test) and International Normalization Ratio (INR). The INR is kept between 2-3. A chart should be maintained by the patient.
- Thrombolytic therapy – in extensive PE when no patient is in shock the TPA (Tissue Plasminogen Antigen) is given especially if right heart strain is present. There is a higher risk of bleeding and is contraindicated if recent surgery has been done or significant trauma is present.
Prognosis – this depends upon
- The underlying health of the patient.
- Size of the PE.
- Cause of the PE.
- The early diagnosis and treatment initiated.
There are over 4 lac cases that are not diagnosed in US each year. Those where the early diagnosis is made the mortality is < 20%. Higher mortality occurs in the elderly, with underlying disease or have a delay in diagnosis.
Prevention of PE
- In hospital setting -compression stocking are routinely used in immobilized patients. Early ambulation is a must in surgery patients and prophylactic dose of LMWH is used.
- During long journey it is recommended to walk every couple of hours.
- Compression stockings are a must if there is a history of previous DVT.
Pulmonary embolism at a glance
- 1. PE is a diagnosis that must be considered in all patients with chest pain and breathlessness and is one of the causes of sudden death.
- 2. The diagnosis of PE is not easy to make and is often missed. Diagnostic strategies need to be individualized to each patient and situation.
- 3. Anticoagulation is the treatment of choice for PE and may be continued for months.
- 4. Prevention is the best treatment for PE which is accomplished by minimizing the risk factors for DVT.