Related FAQ'S
How do you select patients for AV Fistulas?
There should be no arterial insufficiency. A weak pulse means a narrow artery which would reduce the blood flow causing the fistula to fail.
The arm is a preferred site because there are more chances for arteriosclerosis in the leg.
A colour Doppler study is done prior to surgery to make sure that the arteral blood flow is adequate. The vein is viewed to see its size and any blockages.
Fistulas are mostly done under local anesthesia. The patient does not need to be starved and regular medication can be taken.
Am I eligible for dialysis access?
If one has chronic renal failure and needs long term dialysis then access is advised.
Fistulas are avoided if veins are narrowed or scarred from previous line placement or the arteries are blocked.
If AV Fistula is not feasible then AV Grafting is recommended.
Grafts are avoided if there is an ongoing infection. In the unfortunate occurance of infection the grafts must be removed otherwise infection can never be brought under control and the patient could become very sick and septic.
What are the types of dialysis access?
This is a surgical procedure with the portal immediately below your skin.
- AV Fistula – the vascular surgeon joins the artery in your arm to the adjoining vein
- AV Graft – A synthetic tube is placed below the skin connecting the artery to the vein.
In both the cases blood flows from the artery to the vein, dilating it and also strengthing it. By this procedure a large amount of blood passes through the vein rapidly which helps dialysis to proceed efficiently.
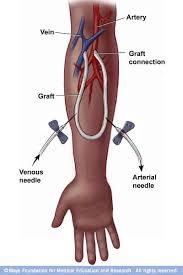
The way AV Fistula is done
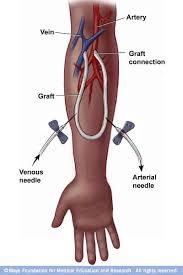
AV Graft placed in the forearm
How is AV Fistula or Graft done?
This is preferably done under local anesthesia unless the patient is very anxious when sedation is given. It is constructed using a single incision at the wrist or the elbow.
The vein is divided and attached to the artery nearby. Some of the blood flowing down the artery to the hand is directed into the vein. Despite the flow of blood in the vein, the flow to the hand is adequate
If the vein is thin and of poor quality or blocked then a synthetic graft is placed between an artery and vein. It is placed as a loop just below the skin in the arm or the forearm and rarely in the leg.
What are the precautions to be taken after AV fistula or graft?
- After the formation of the AV fistula or graft elevate the limb to avoid swelling.
- Keep the incision dry for 48 hours and do not soak or scrub the incision till healed.
- Avoid lifting weights over 7-8 Kg.
- Do not compress the site of surgery by recording blood pressure from that side.
- Report any pain, swelling or bleeding from the site.
- If there is prolonged pain, numbness, coolness or blueness of the fingers or hand please inform your surgeon and much of the blood is being diverted from the hand into the fistula. This is called 'Steal Syndrome'.
- One must perform hand exercise to increase flow of blood into the fistula. This is done by squeezing a soft ball with the hand with fistula.
- Grafts mature in 2-4 weeks but should be used after 6 weeks.
- Grafts have a greater chance to be infected.
- Grafts for 1-2 years which is less than fistulas which could last 3-7 years.
- Till the fistula or graft matures a catheter is used for dialysis.

Steal Syndrome
What are the problems one could face after AV Fistula?
These include:

Aneurysm formation
- Steal syndrome
- Blockage due to clotting
- Narrowing due to stenosis
- Aneurysm formation
- Aneurysm formation
What should I do to stay healthy?
It is important to protect your dialysis access. This is done by:
- Check often to make sure the fistula is working by feeling the vibration known as thrill.
- Monitor the bleeding after dialysis. Should it continue for long take advice.
- Avoid carrying heavy articles in the hand with venous access.
- Do not sleep on the arm with the access.
- Do not wear constricting clothing or jewelry on the arm with the access.
- Do not allow anyone to draw blood or take blood pressure from that arm.
- Do not allow anyone to give injections into the fistula or the graft.
- Keep the site of the fistula or graft clean.
- After each dialysis look for redness or swelling which are signs of infection.
- Do not apply any cream or lotion over the site of the fistula or graft.
What are my choices to undergo dialysis and how do I decide?
The patient has basically three choices:
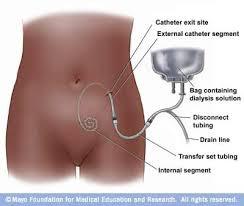
- Peritoneal dialysis
- Catheter placement
- Vascualr access surgery
How is the peritoneal dialysis (PD) catheter inserted?
Peritoneal dialysis
It is done under general anesthesia as a day case. The PD catheter is the length of a ruler and the width of a pencil. During surgery one end is placed in the peritoneal cavity and the rest of the catheter lies outside the abdomen thoiugh it is tunnelled below the skin.
There are two ways of placing the catheter – laproscopic or surgical. In the former two toney incitions are made under genral anesthesia – one for the scope and the second for the catheter. In surgery an incisioni is made and the catheter is placed in the abdominal cavity. It is tunnelled under the skin to avoid infection.
Infection is prevented by using a tube with a valve at the end which is used to close and open the catheter during the exchnage process to avoid infection.
How is the hemodialysis fistula made?
- One of your arteries is connected to one of your veins.
- The fistula takes 3-6 months to mature
- An ultrasound of the veins maybe needed to see its size
- It is performed under local anesthesia and perhaps sedation
What are the post-operative precautions?
- You would have to elevate the limb to reduce the swelling
- You may need pain killers after the surgery
- To strengthen the fistula you may have to exercise the limb by sqeezing rubber ball.
What are the benefits of an AV Fistula?
- Low risk of infection
- Low risk of clot formation
- Performs better than grafts
- Allows greater blood flow
- Lasts longer if cared for – even decades
What are the drawbacks of AV fistulas?
- Bulging veins at access sites
- Take too long to mature
- Rarely they do not mature
How are AV Grafts placed in hemodyalysis?
- This is recommended of the veins are blocked or too small in calibre.
- Synthetic tube is inserted in your arm and connected artery to vein.
- These grafts can be used within 2 – 6 weeks.
How does one plan for vascular access?
- Preserve veins for vascular access well in advance when GFR is less than 30 ml/min.
- The preferred site is radio-cephalic AV fistula.
- Non-dominant upper limb must never be used for drawing blood or IV punctures.
- If the arm for the fistula has to be used then use the hand veins and sites are rotated frequently.
- The preferred access is AV fistula, followed by AV graft and finally central venous catheters.
- Chances of infection are most in central venous catheters followed by AV Grafts and then AV fistulas.
- AV fistula has a better survival than AV Graft.
- Studies show an equal survival on peritioneal dialysis and hemodialysis. Thus peritonel dialysis is preferred to central venous lines.
- The preferred site is radio-cephalic followed by brachio-cephalic fistula.
- If not possible then brachio-basilic fistula is performed followed by transposition 6 weeks later.
- For AV Grafting the preferred site is loop radiocephalic graft or brachio-axillary graft. The least preferred site is the thigh grafts.
When are venograms recommended?
- Oedema in the limb here fistula is planned.
- Accessory vein enlargement in any planned access site.
- Differential extremity size if it is planned as access site.
- Central line in subclavian vein in the planned side.
- Previous arm neck or chest injury or surgery on the venous system of the planned side.
- Pacemaker in the venous drainage of the planned side.
- Multiple previous accesses on the planned side.
What is the best timing for AV access, its placement and its maturation?
- Fistula is advised when the GFR is 15-20 ml/min and there is progressive renal disease.
- It is important to make the fistula 3-4 months before the anticipated use of the fistula.
- AV grafting is recommended when it is not possible to use an AV Fistula and is done 3-6 weeks before the anticipated use.
- Permachaths are put immediately before the dialysis as they need no time to mature. However there is a chance of infection, thrombosis, and dialysis inadequacy. The tip must be beyond the SVC in the right atrium which is confirmed by radiography. Insertion is guided by ultrasound to avoid complications.
- Subclavian access is used only when jugular access is not possible.
- Avoid subclavian or jugular catheters on the side AV fistula is maturing.
- The patients with chronic renal disease needing acute hemodialysis vascular access use percutaneous inserted catheters. They are inserted just before use.
- Femoral catheters must be at least 19 cm long to reduce recirculation. They are left so along as there are no complications.
- AV fistula maturation depends upon the size of the artery, the vein and the cardiac output. The time of use depends upon clinical judgment.
How can we enhance the use of AV Fistulas?
- Arm and hand exercises by squeezing a rubber ball with lightly applied tourniquet.
- Selective tying of the major veins side branches.
- Rest till the swelling has resolved.
- AV Graft should not be cannulated till the swelling is reduced and the graft is palpable along its course. This takes 3-6 weeks.
- Never cannulate a graft within 2 weeks of making.
- If the swelling does not respond to elevtion or persists beyond 2 weeks of placement use venogram or non-invasive study to evaluate central veins.
How is the functioning of the vascular access monitored and maintained?
- Measure the access flow bimonthly in case of AV Fistula and venous pressure or access flow monthly in AV graft.
- Perform angiography of the fistula flow falls below 500ml/min and AV Graft below 650 ml/min.
- Intra-access flow and monitoring changes in flow.
- Static venous pressure.
- Dynamic venous pressure.
- Slow flow venous pressure.
- Using access recirculation measures one must be aware that the recirculation is abnormal and has to be investigated. Recirculation of > 5% using non-urea based measures or > 15% using urea based methods significant and needs angiography.
- Unexplained reduction in the form of hemodialysis delivered.
- Persistent swelling of the arm with AV graft.
- Prolonged bleeding after removing the needle or altered thrill in the graft.
- Increased negative arterial pre-pump pressure that prevents increasing to acceptable blood flow.
- Venography or Doppler ultrasound.
How are poorly functioning venous access managed?
Any finding of access dysfunction using any technique must be investigated by an angiogram and corrective measures taken – angioplasty or surgery.
In the period before corrective measures can be undertaken because the dialysis circuit exceeds the access flow, access recirculation leads to inadequate dialysis. If this occurs then the dialyser flow is reduced to below measured access flow.
How to prevent infection in vascular access?
- Teach patients and staff on infection control.
- Change dressing each time after dialysis using gauze and povidon iodine ointment.
- Catheter care and measuring flow is done in the sterile way.
- Catheter connection and disconnection is done in a sterile way wearing gloves and mask.
- By this technique trials showed a significant reduction in stapholococcusaurius, reduced incidence of bacteremia and catheter tip colonization.
How do we manage vascular access complications?
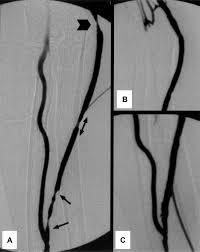
- Use of angioplasty in significant stenosis of AV Fistula or AV graft. If this is not possible then revision is done.
- In AV fistula aneurysm intervene only of the overlying skin is compromised or the aneurysm is expanding or there are limited puncture sites.
- AV graft surgery is done if the graft is degenerated or pseudo-aneurysm is present.
- Correct the thrombosis of the AV graft with thrombolysis or surgical thrombectomy.
- The commonest site of stenosis or thrombosis is near the AV anastomosis.
- AV Fistula stenosis and angioplasty.
- After correction the parameters should return to within normal limits of patency.
AV Fistula stenosis and angioplasty
When do we call it reasonable patency?
The goals of reasonable patency in the absence of thrombosis are:
- After Angioplasty – 50% unassisted patency at 6 months. No more than 30% residual stenosis after the procedure and resolution of physical indicators of stenosis.
- After surgical revision: 50% unassisted patency at 1 year.
- If angioplasty is needed more than 2 times in 3 months then surgical revision is considered.
Stents are useful in selected cases when angioplasty fails:
- Central venous stenosis
- Limited residual access sites
- Surgical inaccessable lesion
- Contraindication to surgery

Angioplasty for AV Graft stenosis
Thrombosis should be corrected within 24 hours and the venous access then evaluated for a stenosis by doing a fistulogram. Outflow venous stenosis is presnt in > 85% of the thrombosis in AV grafts. Angioplasty or surgical correction is performed.
Are there any problems after thrombolysis?
- Thrombolysis followed by angioplasty – 40% unassisted potency at 3 months.
- Surgical thrombectomy and revision – 50% unassisted patency at 6 months and 40% at 1 year.
- Immediate patency 85% in both techniques.
- The use of aspirin or wafarin in graft and fistula thrombosis has not been very encouraging.
- Treat hand ischemia due to arterial steal with distal revascularization along with internal ligation procedure. If not possible then ligation of AV graft or AV fistula.
- Treat central vein thrombsis with angioplasty and stenting if necessary.
- Thrombosed hemodialysis catheters are treated with tPA.
How is steal syndrome treated?

Severe ischemia hand with gangrene finger
Significant hand ischemia occurs in 2-8% after AV access Risk factors are:
- Female sex
- >60 years
- Diabetes
- Use of brachial artery as donor site
- Severe ischemia hand with gangrene finger
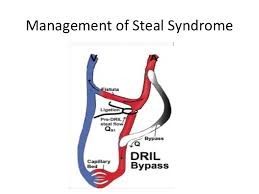
Bypass for steal syndrome
Treatment is by ligating the artery distal to the fistula site and a short bypass from proximal to the inflow of AV access till just diatal to the ligation. Immediate releif of the symptoms occured and 1 year patency was 70%

Arm swelling in central vein occlusion
Central vein stenosis may cause marked limb swelling with AV access on the same side. Percutaneous angioplasty is helpful and if this repeatedly occurs then a stent is placed.
What are dysfunctional hemodialysis catheters?
This is failure to perform hemodialysis based on catheter related thrombotic or mechanical factors. It could be due to the formation of a fibrin sheath within the catheter which acts as a nidus for thrombosis. tPA can restore the patency. 2 mg of tPA in each lumen for 24 hours makes them patent in 80%. If there is a contraindication to the use of tPA then the catheter needs to be changed over a guide wire or the fibrin sheath stripped.
What is the role of antibiotics in infected venous access?
- Treat extensive infection of the AV Graft with parenteral antibiotics and graft excision.
- Treat infections of the primary AV fistulas as subacute endocarditis with 6 weeks antibiotics.
- Treat Central venous catheters related bacteria with systemic antibiotics and catheter exchange over a guide wire.
- Treat central tunnel infection without bacteremia with systemic antibiotics na appropriate local measures. Remove catheter if it fails to resolve in 2 weeks of therapy.
- Central venous catheters are associated with a significantly higher risk of bacteremia compared to AV Fistulas. With AV Grafts the risk is moderate. The grafts must be removed under systemic antibiotic cover.
- If there is bactemia in any of these venous accesses start wihtbroad spectrum antibiotics like cefazolin along with gentamycin after the drawing of blood cultures. If the patient is allergic to cefazolin then substitute vancomycin.
- The sensitive antibiotics are given for 2-4 weeks.
- Central venous catheters should be removed rather than exchanged over a guide wire if the patient is unstable or symptomatic for over 36 hours.
- New catheter should not be placed until blood culture taken 48 hours after the cessation of antibiotics has been negative.
- If the catheter exit site shows redness, crusting or exudate but no systemic symptoms and negative blood cultures just care for the local site and perhaps oral antibiotics. The catheter need not be removed.
- If infection fails to come under control within 2 weeks despite therapy replace the catheter and place another one at a different site.
What is the quality of care standards in venous access?
- 60% of the venous access would be AV fistulas.
- Rate of Graft thormbosis should be less than 0.5 thrombotic episodes per patient year at risk.
- After the first 2 months the rate of thrombosis should be < 0.25 episodes per patient year at risk.
- The rate of infection should be below 0.01 episode per patient year at risk for primary AV Fistulas and 0.1 episodes per patient year at risk for AV Grafts.
- For tunneled cuffed grafts the target rate of systemic infection is < 0.5 episodes per patient year at risk.
- The primary failure rates for AV Grafts in the forearm straight grafts should be < 15%, < 10% in forearm loop grafts and < 5% in the upper arm grafts.
- The cumulative patency rates for all AV Grafts should be > 70% at one year, > 60% at 2 years and > 50% at 3 years.