Abdominal Aortic Aneurysm
Management of AAA
Dr Nadeem Niyaz Jan
DNB, FRCS
Consultant Vascular Surgeon
Important facts
- Aneurysm – localized irreversible artery dilatation >50%.
- 95% AAA –infra-renal.
- 5-7% incidence population > 60 yrs.
- Commoner in white males - ? why.
- Other atherosclerotic manifestations do not have a racial predilection.
Why does it happen?
- Auto-immune reaction " macrophage activity – T&B lymphocytes invade arterial wall " activate proteolytic activity " degrade elastin & collagen " weaken arterial wall " aneurysm.
- Lowest levels of elastin & collagen in distal aorta just before bifurcation.
Why is it lethal?
- < 4 cm diameter – 10% rupture.
- 4-5 cm diameter – 25% rupture.
- > 6 cm diameter – 50% rupture in 1 year.
- Rupture has a 80% mortality.
- Surgical mortality < 5%.
- life expectancy – dramatically - AAA -1950 – 60 – 8.7 new AAA / 100,000 -1971 – 80 – 36.5 new AAA / 100,000.
Recent concept on rupture AAA
- Old concept – mechanical increase in size < ballooning < thinning of wall < rupture.
- Protein metalloproteinase – 9 - 5 times higher levels in wall of 5-7 cm aneurysms compared to 3-5 cm - break down of collagen within the wall of the aneurysm.
- Confusion regarding life threatening size will end and save many lives.
- Chlamydia pneumonae antigens.
Whom to screen?
- > 60 years.
- Smokers.
- COPD patients.
- Atherosclerotic patients with CAD.
- PHT.
- Family history.
How do they present?
- Mostly asymptomatic – 75%.
- Compression – bowel, ureter.
- Peripheral emboli.
- Back or abdo. Pain unreleaved by position.
- Shock – 20%.
- pulsatile abdomen mass left of midline between xyphoid & umbilicus – knees bent & during exhailing – 50% accuracy.
What investigations do I order and why?
- Plain AXR - AP + Lat – calcification –eggshell appearance seen in < 50% cases –This is not the first investigation.
- Ultrasound - initial test – presence & size – Gas and obesity hinder proper diagnosis – can’t detect leaks, rupture, branch artery and suprarenal involvement - ideal for screening patients.
Can AAA be Tt conservatively?
- Acute reduction in BP & pain killers.
- IV sodium nitroprusside.
- IV Beta-blockers – esmalol, labetalol, propranolol, metoprololv.
- BP maintained 100-120mmHg systolic.
- Beta-blockers – maintain HR – 60-80/min.
- Morphine sulphate IV for pain.
When to intervene?
- Aneurysm – rupture or suspected.
- Symptomatic or rapidly expanding.
- > 4 cm diameter.
- Complicated – embolism, occlusion.
- Atypical aneurysms – dissection, mycotic, seccular or inflammatory.
What should I tell relatives?
- Pre-hospital rupture – >50% die on way.
- Those who reach – mortality # 1%/min.
- Prognosis good - not in severe shock on arrival – get immediate resuscitation & surgical intervention.
- Fatal MI – elective repair – 4.7%.
- Non-fatal MI – elective repair – 16%.
Traditional Vs Endovascular graft
| FEATURE | TRADITIONAL | ENDOVASCULAR |
|---|---|---|
Invasiveness | Abdominal Surgery | Minimally Invasive |
Incision | Epigastrium-pubic symph. | Bilat. Groin |
Anaesthesia | 4-6 hrs GA | 2-3 hrs epidural |
Operative time | 3-4 hrs. | 2-3 hrs |
Length of stay | 5-10 days | 1-3 days |
Traditional Vs Endovascular graft 2
| FEATURE | TRADITIONAL | ENDOVASCULAR |
|---|---|---|
Activity | Limited in week 1 | Anbulatory on day 1 |
Blood Transfusion | Loss 1200-2900ml chance | Loss 200-600ml chance |
Ventilation | 1st day must | Only mask |
Mortality | 3-5% | 1-2% |
Patient satisfaction | Lower-pain, energy level | High - minimal disconfort |
How safe is traditional surgery?
- Mortality. < 5% - relatively safe
- Peri-operative MI.
- Hemorrhage.
- Renal failure
- Post-op ileus, bowel obstruction, ischemic colitis.
- Spinal cord ischemia.
- Lower limb ischemia - emboli.
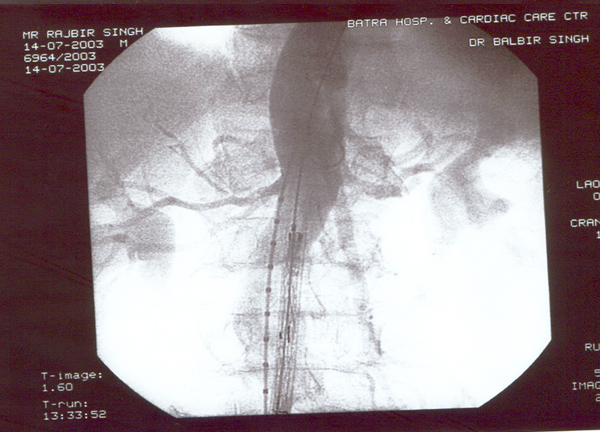
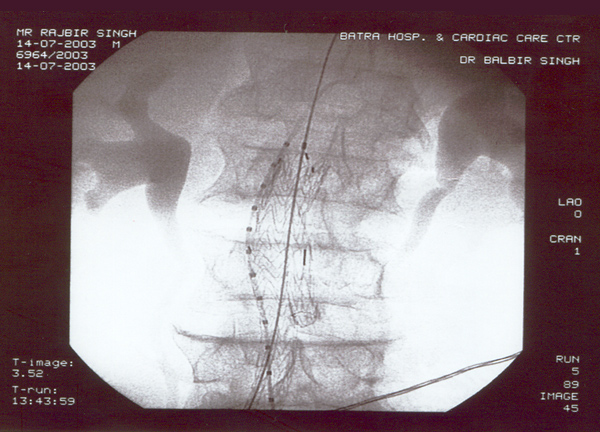
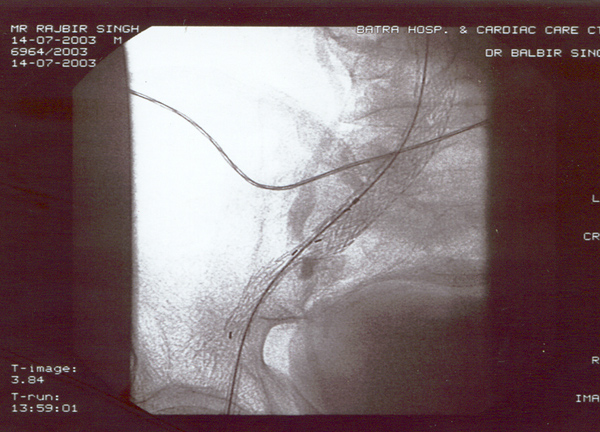
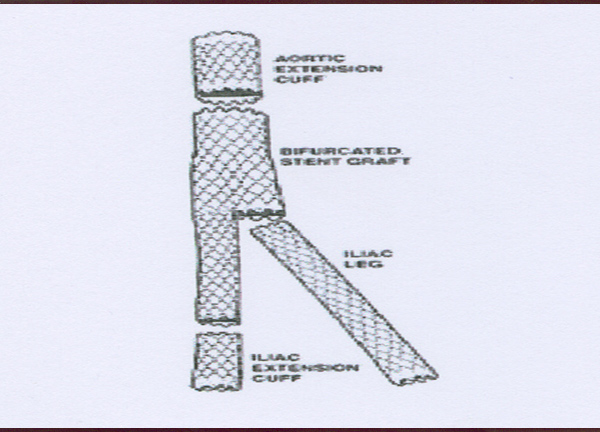
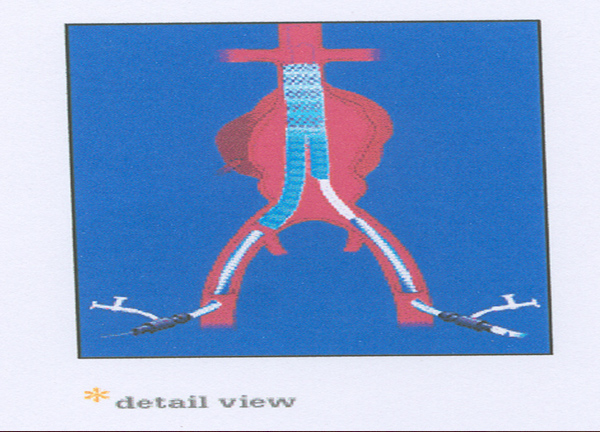
Is endovascular grafting possible?
- Greatest mural diameter.
- Extent of aneurysm – proximal & distal necks + extension into iliacs.
- Tortuosity of aorta & intramural thrombus.
- Iliac anatomy – occlusion; IIA relation to aneurysm, size & tortuousity.
- Calcification of neck and iliacs.
- Femorals – calcification or occlusion.
Who qualifies for endovascular grafting?
- > 21 years – for written consent.
- Radiation exposure – postmenopausal or surgically sterile women.
- Anesthetic clearance.
- Life expectancy > 2 years.
- Pre-op angio – IMA not essential for intestinal perfusion.
- One IIA must be preserved – rectal flow.
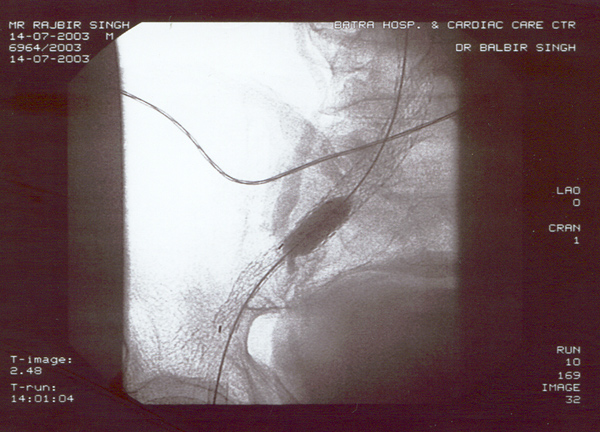
This too has a learning curve.
- Peri-graft leaks - 8- 44%.
- Graft limb thrombosis – 1–10%.
- Renal artery occlusion – 6–12%.
- Femoral artery injury – 2-17%.
- Hemorrhage - 2-17%.
- Graft dysfunction - 6-23%.
- Graft deployment failure - 2-12%.
- Graft malposition - 2-20%.
How good are interventionalists today?
- Recent study – 50 cases – 47 (94%) successful – 3 conversion to open surgery.
- Perigrafts leaks – 33% - resolved spontaneously or coil insertion.
- 3 had graft occlusion – thrombolytic therapy successful.
Investigations in FU
- Conventional surgery – yearly with US.
- Endovascular grafting – Immediate post-op with CT 6 month after yearly.
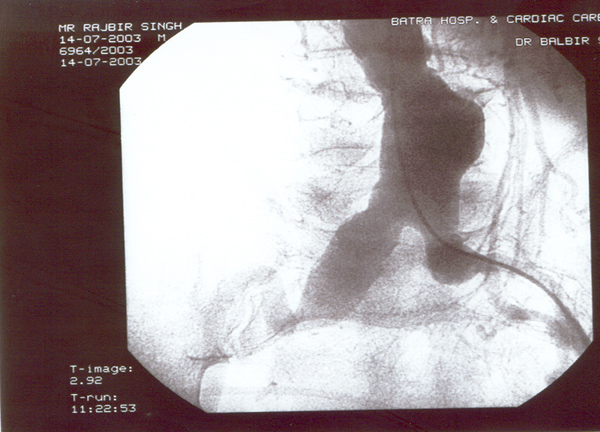
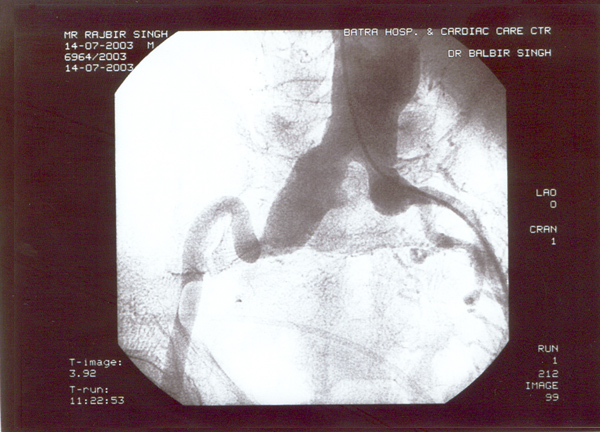
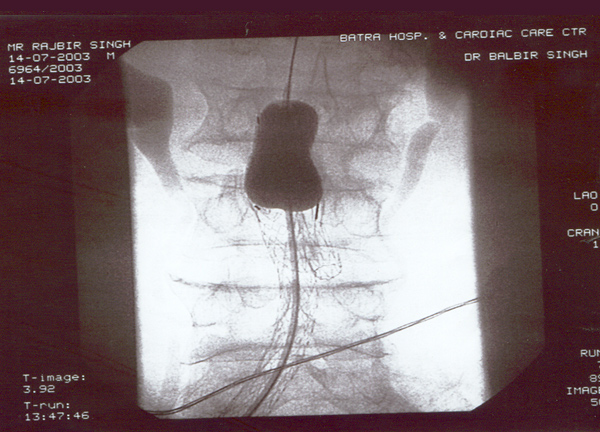
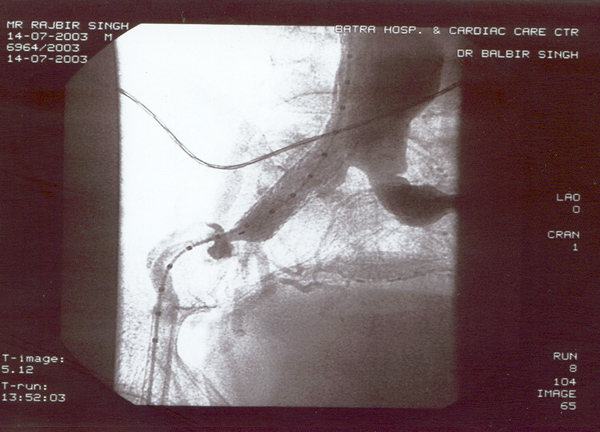
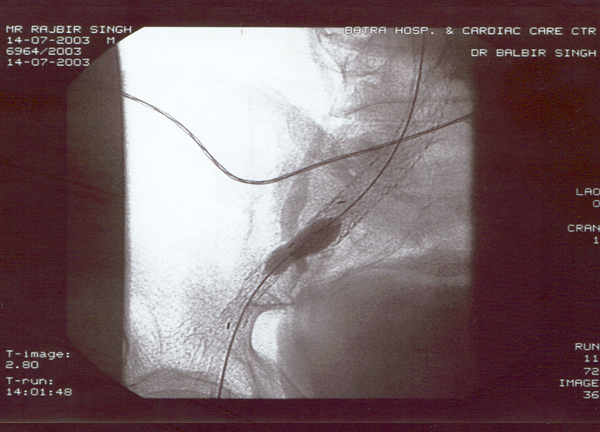
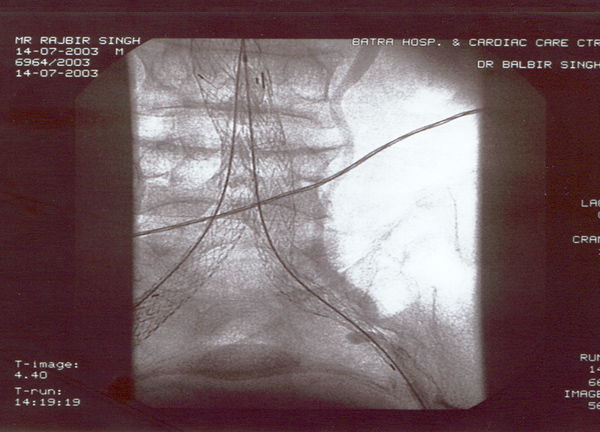
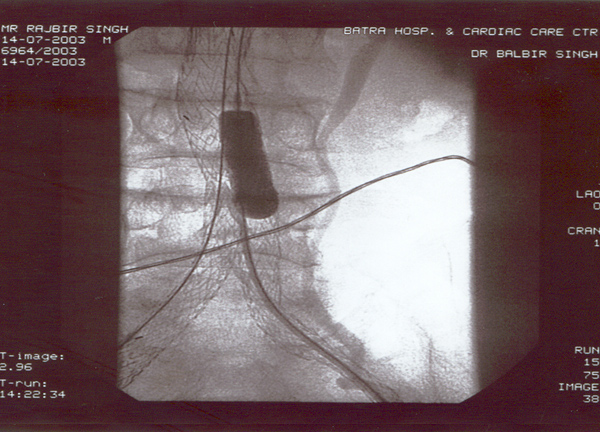
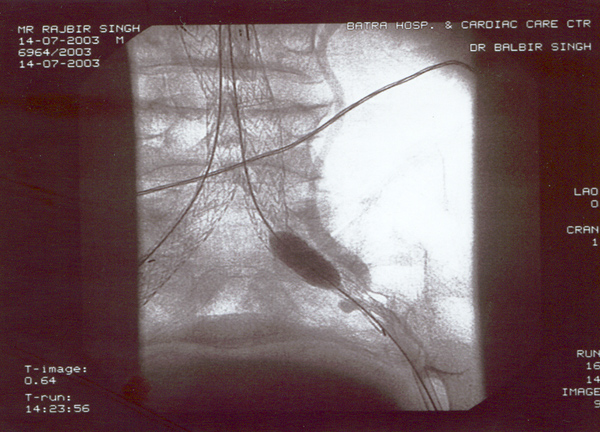
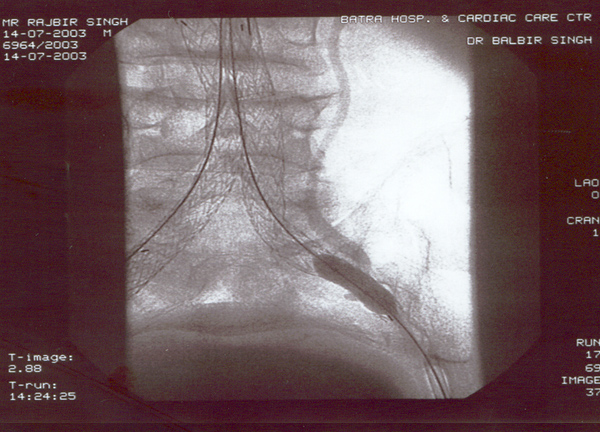
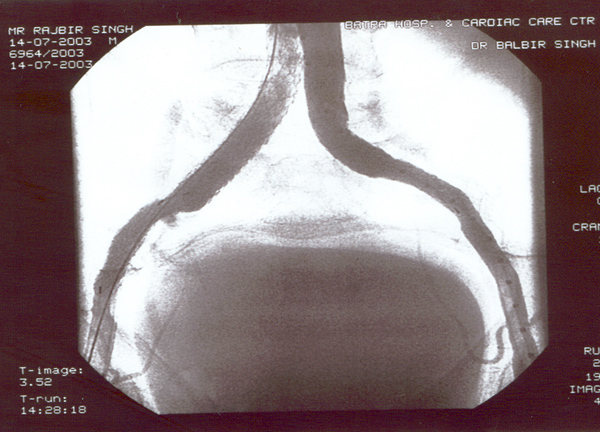
Case presentation
- Rajbir Singh, 60 yrs male.
- Abdominal pain for years now worsening.
- Severe COPD + PHT + CAD.
- USS abdomen for abdo pain – 7cm AAA.
- Pulsatile abdominal mass – non tender.
- All peripheral pulses palpable to ankles.
- No complications – blue toe syndrome.